- 21/04/2021
- Dr. Samrat Jankar
- 0 Comments
- Blog
Diverticular disease of colon in Indian population
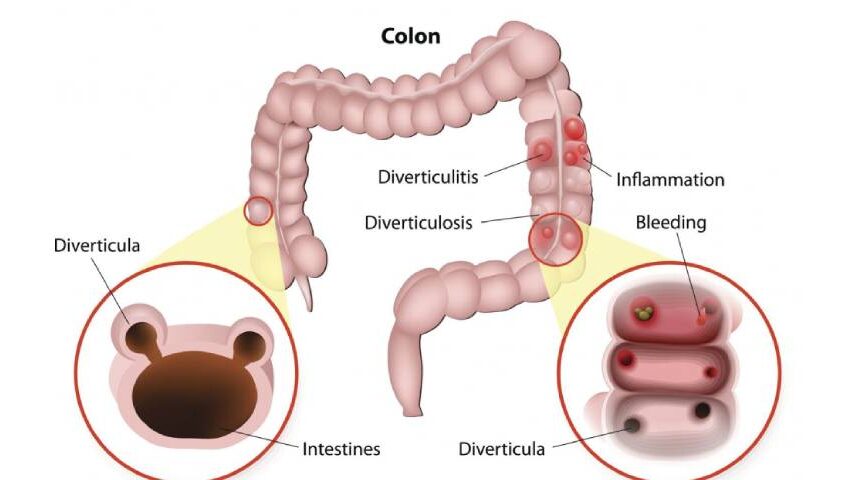
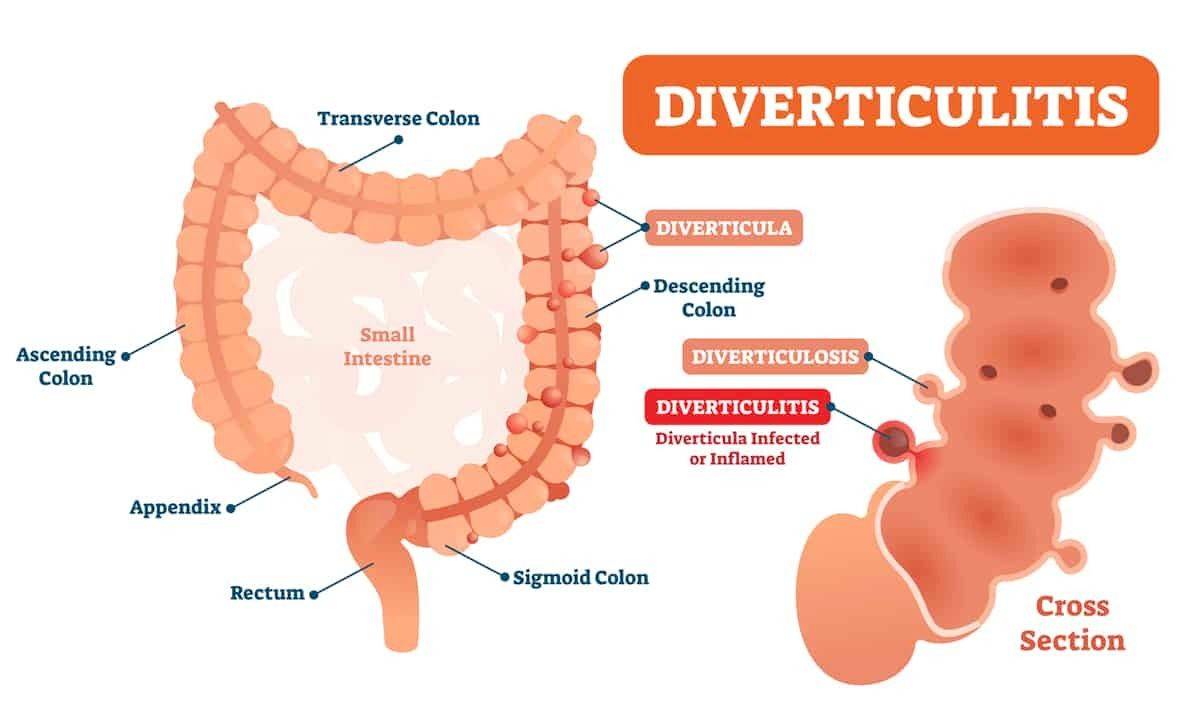
What is diverticulosis and diverticulitis?
What’s the difference between diverticulosis and diverticulitis?
Diverticulosis is simply the presence of these tiny bulges or pockets (diverticula) in your colon. They usually don’t cause any symptoms or need to be treated.
Diverticulitis is inflammation (swelling) and infection in one or more diverticula. You may feel pain, nausea, fever and have other symptoms. This is a much more serious and potentially a dangerous condition.
How common is diverticulosis in Indian population?
Who is most likely to get diverticular disease?
You are at increased risk of diverticular disease (diverticulosis or diverticulitis) if you are :
- Over 40 years of age.
- Male.
- Overweight.
- Eating a low-fiber diet. If you don’t eat a lot of fruits, vegetables, beans and legumes, breads and grains or nuts.
- Eating a diet high in fat and more of red meat.
- Not exercising.
- Taking NSAIDs(frequent painkillers)
- Smoking
What causes diverticulosis and diverticulitis?
What are the symptoms of diverticulitis?
The symptoms of diverticulitis include:
- Pain left lower side of your abdomen is the most common symptom
- Fever.
- Chills.
- Cramps in the lower abdomen.
- Nausea and/or vomiting
- Constipation
How is diverticulitis diagnosed?
- Blood test: Your blood is checked for signs of infection, such as a high WBC counts
- Stool sample: Your stool sample is checked for the presence of abnormal bacteria or parasites to rule out infective cause
- CT scan: A CT Sacn abdomen and pelvis can show infected or inflamed diverticula and also reveal the severity of diverticulitis.
- Colonoscopy: In this exam, the full length of your colon can be examined. A thin, flexible, lighted tube with a camera, called a colonoscope, is inserted through your rectum and into your colon. During a colonoscopy, your colon is checked for abnormal growths, ulcers, bleeding or other problems that could cause changes in bowel habits or abdominal pain. It is very important in long-standing cases to rule out any cancer.
How is diverticulitis treated?
If your diverticulitis is mild, consult Dr. Samrat Jankar, an experienced laparoscopic surgeon in Pune, he will prescribe an oral antibiotic and mother symptomatic medications. Initially rest and liquid diet will be recommended until your symptoms improve. Once your symptoms improve, you can slowly return to soft foods, then a more normal diet(high-fiber).
If your diverticulitis is severe, you have rectal bleeding or are having a repeat bout of diverticulitis, you may be admitted to the hospital to receive intravenous (IV) antibiotics, IV fluids or possibly be considered for surgery by Dr Samrat Jankar, if associated with complications.
What does the surgery for diverticulitis includes?
Surgery usually involves removing affected part of the colon. During surgery, the diseased section of the colon is removed and the colon is reattached to the rectum.
Depending on the extent and severity of disease, surgery can be performed in a single surgery, in two surgeries, in an open procedure (tradition surgery performed through a large incision) or by a minimally invasive laparoscopic procedure (surgery performed through small holes in your abdomen). Dr Samrat Jankar, an experienced laparoscopic and colorectal surgeon based in Pune does almost all diverticular disease surgery by laparoscopy except few where safety comprmised.
You may or may not need a colostomy in certain complications. The colostomy bag may be needed for several months while your colon heals. Once healed, the colon is reattached to the rectum (at which time the colostomy bag is removed).
Tips to avoid prevent diverticulosis?
To accomplish this:
Eat more fiber: Fiber pulls more water into stool, making it bulkier, softer and easier to move without any straining for defecation.
Drink plenty of water: Eating more fiber absorbs more water, so you’ll need to increase the amount of water you drink to keep stool soft. It is recommended to drink at least 3 to 4 liters of water every day.
Exercise daily: Physical movement helps food pass through your intestinal system. Exercise for 30 to 45 minutes on most days if you can will help to regularize stool pattern.
What foods are high in fiber?
High-fiber foods include:
- Vegetables, such as broccoli, cabbage, spinach, carrots, asparagus, squash and beans.
- Brown rice.
- Bran products, made from rice, corn, wheat, oats, barley rye and millet.
- Cooked peas and beans.
What should I expect if I have been diagnosed with diverticular disease?
If you’ve been told you have diverticulosis, this is usually not a cause for concern. This condition is very common and increases with age. You likely won’t even have symptoms if you have diverticulosis.
Up to 30% of people with diverticulosis develop diverticulitis. Between 5% and 15% will develop rectal bleeding.
Most people who have diverticulitis will recover with about a seven to 10-day course of antibiotics and rest. Severe complication of diverticulitis occur in about the following percent of people: perforation of the colon (1% to 2% of patients), obstruction (rare), fistula (14%) or abscess (30%).
